Belly Fat Removal Without Procedure: Safe and Proven Methods
Introduction
We welcome you to the realm of the latest technologies and trends of non-surgical belly removal, where we get your desired body shape. Everyone thinks that maintaining a body figure by losing fat is more challenging, but all these are myths. We drag you to the world of body sculpting, which is accessible. If we take a look at the previous, the process was challenging and complex to achieve belly fat removal without surgery. This process has gained a significant approach from the person who is facing body shaming and wants belly fat reduction. Non-surgical procedures for belly fat removal are easy to apply, and this approach has many alternatives. These removal methods provide productive results in achieving body sculpting.

Various fat reduction procedures are in practice for the well-being. First, anyone must want to reduce belly fat or adopt belly fat removal surgery. The answer to this query is based on various factors; the top concern is beauty. Other may include the increased risks of diseases due to the over-production of belly fats. Therefore, the most convenient solutions will be applied to reduce belly fat, and solutions will be tailored to the patient’s conditions. These practical methods help you to gain a perfect figure. We will discuss each belly fat removal method in detail, including all interventions and perks of the applied procedure within the comfort zone of every individual. No doubt, each non-surgical belly fat removal is cost-effective and budget-friendly.
Advantages of Non-surgical Body Contouring
Let's embark on a journey with us if you want to know the perks and challenges of these non-surgical body contouring procedures.
1. Non-invasiveness
The most beneficial aspect of non-surgical body contouring is that there is no need to induce anesthesia or require excision of fat removal. This surgical intervention has no complications or risks and securely removes excess body fats through different non-surgical procedures.
2. Less discomfort
These body contouring treatments are performed within the patient's comfort zone, so he will soon return to his routine. Conversely, surgical treatments are more painful, as inclusions or cuts may be produced, and require a much longer time to cure and return to normal physical activities. Thus, non-surgical body contouring provides a flexible and convenient healing procedure.
3. Targeted belly fat removal
As you already know, non-surgical belly fat reduction is targeted, which means only specific fat sites will be removed, such as from the abdomen, thighs, arms, or hips. This precise belly fat removal performs proper body sculpting. Another perk of targeted removal is that it cannot harm the surrounding tissues and organs.
4. Organic results
Did you know body fat removal produces organic results? What does it mean? It is a way of making the body look natural as if it had no fats before. Although non-surgical treatments are slow in producing organic results, the outcomes will be permanent and promote more natural body contouring. Surgical procedures are diverse but do not produce a natural look, and variations in the body may appear artificial.
5. Reduced complications and potential risks
As non-surgical belly fat removal does not require any surgical method, it can proceed quickly without producing any potential risks or complications. This treatment will protect the organs or skin from infectious attacks or adverse situations. Also, if any patient experiences discomfort or bruises, he will recover soon with proper and effective medications.
6. Adaptability
Another advantage of fat removal without surgery is that the procedure is versatile and carried out according to the patient’s will. It's up to the individual how much and from which area he wants to get fat reduction. In other words, non-surgical fat removal is a personalized phenomenon in which the patient can achieve treatment according to his choice to improve body contours and appearance.
Overall, the advantages of non-surgical body contouring are mind-blowing and flawless for any individual. These are the most convenient and alternative methods to get body fats quickly with less struggle. Your body physique will be maintained after such treatment, and you will get enhanced body sculpting.

Types of Fat removal from various organs
Fat removal procedures, or non-invasive lipo, can be performed on various organs. Each organ fat removal has different strategies, depending on the amount of fat deposition. The foremost organ that makes everyone conscious about their weight is belly fat. Belly fats are the primary reason for the decrease in the body’s beauty and the destruction of the whole figure. Most of the fat deposition takes place in this area. Increased belly fats cause the stomach appearance to become flatter. But you do not need to worry as each type of fat removal is accessible and has commonly targeted processing. Let’s take a comprehensive view of types of fat removal from various organs:
1. Subcutaneous fats
As the name shows, these fats are present below the skin surface in various organs such as the abdomen, thighs, arms, and hips. The function of this fat is to protect the organs and maintain body temperature. It protects the form of insulation and energy reservation.
2. Visceral fats
These fats are deep inside the organs and primarily present in internal cavities such as the abdominal cavity, liver, pancreas, or intestines. Their mode of action is to enhance metabolism and hormonal regulation. However, the risk factor of visceral fats is that they cause chronic heart conditions and diabetes if their volume increases.
3. White fats
White fats are the usual body fats present within the whole body, surrounding tissues, and organs. They are mainly present in adipose tissue, providing an energy source when there is a shortage. The availability of energy is present in the form of triglycerides. These fats also enable the release of hormones that facilitate hormonal regulation.
4. Perivascular fats
As the name suggests, they are around the vascular system, such as arteries and veins. Their function is to regulate the action of blood vessels and induce inflammation associated with atherosclerosis.
5. Epicardial fats
Epicardial fats surround the heart tissues to protect the significant pumping organ. These fats are present in the form of a uniform layer between two barriers of the heart: the pericardium and epicardium. The purpose of epicardial fats is to act like a cushion and preserve the heart in the perfect place. However, an increase in epicardial fats increases the risk of heart attacks.
6. Intramuscular fats
These intramuscular fats are present in muscles throughout the body. They also provide energy to muscles for movement and movement, and the fat level fluctuates depending on the muscle requirements.
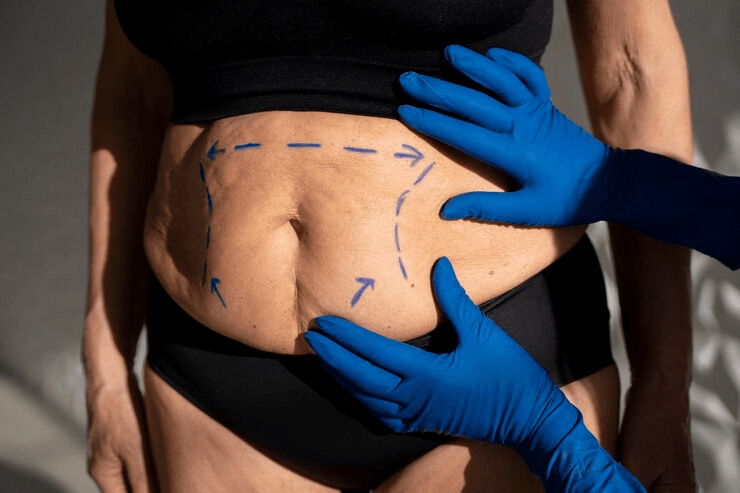
Non-surgical procedures for Belly fat removal
Although non-surgical belly fat removal treatments traditional to proceed with excessive fat removal, they are an utmost step to enhance body figure and avoid invasive procedures. These successful procedures efficiently remove extra body fats without passing through invasive techniques. Non-surgical fat removal has many perks; we will discuss them with application strategies. The purpose is to make people aware of these non-invasive procedures.

1. Cryolipolysis
The word originated from the freezing phenomenon; here, cryolipolysis is an excellent non-invasive treatment and is highly utilized worldwide. The purpose is to target the extra belly fats and remove them to look like a sculpting body. The sculpting body is obtained by freezing the fat cells in the abdominal area. Let us understand some of its working procedures. The treatment is carried out with the help of a specialized applicator applied to the skin, which promotes the cooling process of freezing and thereby destroying fat cells without damaging surrounding tissues. Within a few weeks, the body becomes natural and eradicates the previous extra fat cells. This effect will cause fat reduction and enhanced body contouring. The cryolipolysis is approved by medical health science and produces productive results in decreasing belly fat. It is a personalized treatment based on individual fat reduction aims due to apoptosis. Once the fat cells die, they will be eliminated from the body through the lymphatic system. The plus point is that bed rest is unnecessary, and the patient moves into the everyday routine. You can get the optimal results 1 to 3 months after the treatment, but the recovery will occur in a few days or weeks.
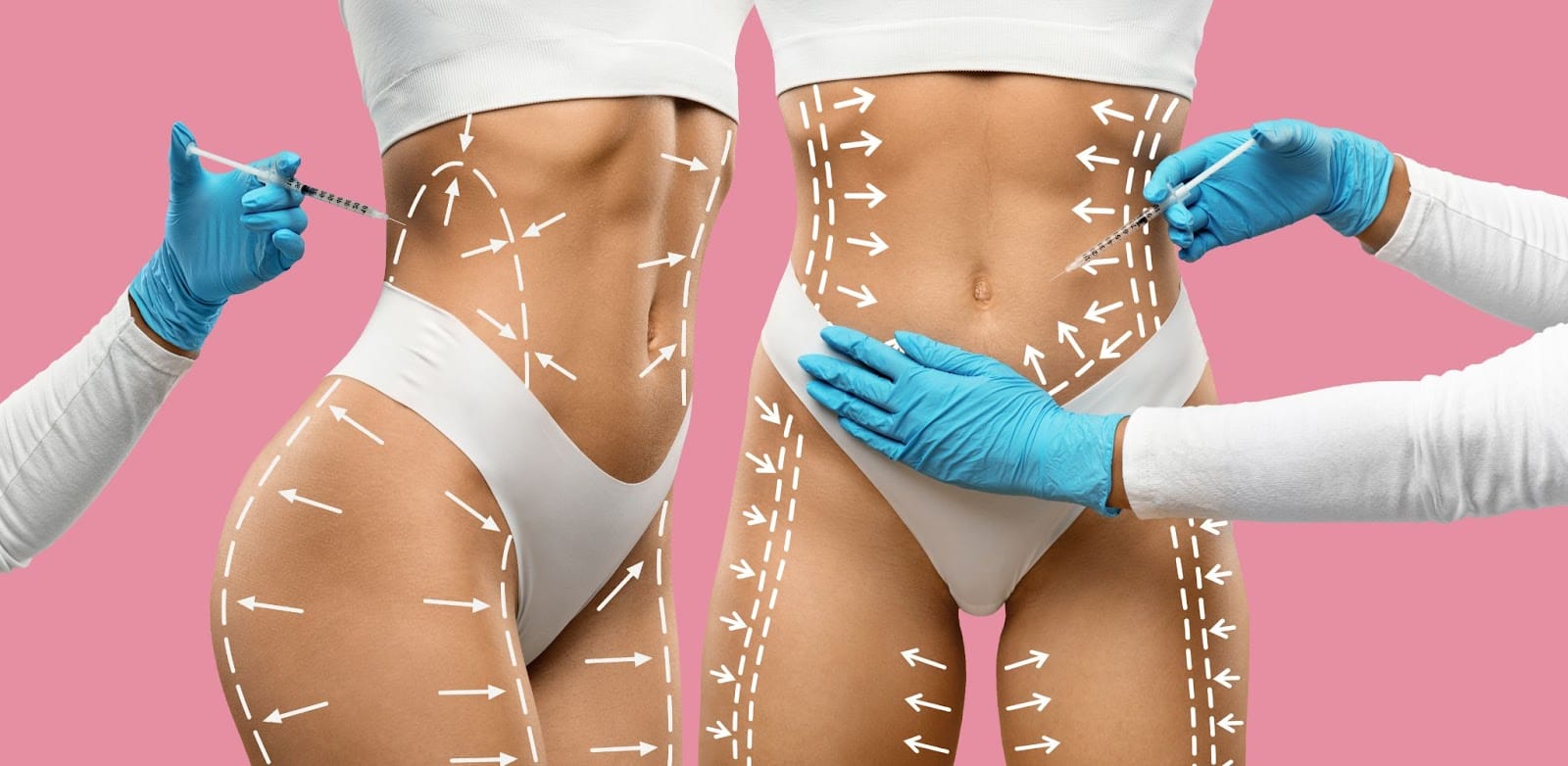
2. SculpSure
Another prominent non-surgical body contouring treatment is sculpture. Sculpsure is the latest and new invention of technology that uses laser treatment to remove excess fats from the body. This laser treatment can be applied to various organs, such as the ankle, abdomen, thigh, lower chin, and back for fat reduction. Before we can begin the treatment, it's essential to have a thorough and detailed consultation. Don't stress about any possible side effects from the laser sculpting process. Just focus on getting the best care possible for you. Different and fixed applicators promote this service in the targeted areas. The laser will increase the temperature of those areas and cause the fats to burn rapidly. It is a heating process that does not harm the body or surrounding tissues; it just burns the targeted fat areas. During the treatment, the fat due to extreme warmness will cause cell death due to apoptosis. The natural process of lymphatic cells continues to remove these dead cells. After the laser session, you can return to routine promptly as SculpSure requires no long duration for recovery. Some patients may face potential but temporary side effects such as inflammation, swelling, or itching for only a few days. These conditions will not last long. Patients will seek visible outcomes in a maximum of 12 months, but the outcomes will be permanent. Sculpsure laser treatment is suitable for all skin types and areas with more fats and cannot be reduced by controlling diet and exercise. This non-surgical fat removal is productive worldwide without local anesthesia and related agents.
3. HIFEM treatment
High-Intensity Focused Electromagnetic (HIFEM) technology is a highly efficient and revolutionized body contouring treatment known as Emsculp. Its purpose is to remove extra fats from muscle mass and other targeted areas such as the abdomen, thigh, arms, and hips. The procedure will be carried out by high-intensity electromagnetic radiation that passes through the skin deep down and causes a reduction in body fats. In the first step, muscle activation will take place. Then, muscle contraction will be produced due to the high energy source. The muscle contraction is more than achieved through regular exercise. Extreme contraction is associated with muscle adaptation and remodeling. Due to this activity, muscle strength increases. The muscle adaption through HIFEM energy causes metabolic changes that lead to apoptosis. The apoptosis will break down the targeted fats in the areas, reducing that. HIFEM has a dual nature, which is dual functionality; one is to reduce body fats, and the other is to build muscle to get proper and figured body contouring. The therapy is not painful, and the patient will achieve a normal state after 30 minutes. HIEM provides prominent improvements in body contouring with non-surgical treatment.

4. Ultrasound Cavitation
Ultrasonic cavitation is another technology that improves body contouring through non-surgical fat removal. This technique uses ultrasonic waves to reduce fats by burning fatty tissues. Ultrasonic waves will fall on the targeted deposited fats so that stubborn fat cells will remove. The targeted application of waves breaks the fat cells, but make sure the waves are low-frequency to get harmless outcomes. The ultrasonic cavitation will proceed through proper consultation from a medical health provider as the assessment is necessary, either it is beneficial for you or not. Let’s go over this procedure and how it works.
The ultrasonic device falls the waves on the targeted portion for this treatment. Ensure the fall will be targeted as it may damage the surrounding tissues. The waves pass down beneath the skin layers and affect the fat cells. The surrounding tissues will be in their original state. The cavitation will be produced by this means. It means that fat cells start vibrating by disturbing their integrity, and tiny air bubbles are created. The fats will convert into low-intensity triglycerides and fatty acids. Results from this treatment can be achieved gradually but are permanent.
5. T-shape
The T-shape fat reduction process involves various therapies, all non-surgical procedures. It is the best opportunity to get non-surgical body contouring with these therapies, including mechanical massage, vacuum therapy, and other treatment plans. In a vacuum, the lymphatic system improves to eliminate extra fats. Rapid drainage will promote the large amount of fatty tissues and fat cells to get out from the body. Mechanical massage also enhances blood circulation, facilitating fast and effective means for fat removal and toxins. Sometimes, customized treatment plans effectively reduce fat, but a profound examination is necessary. Topical customized treatment plans will only work in some individuals and depend on fat reduction goals.
6. HIFU
High-intensity focused ultrasonic technology effectively removes non-surgical fat from different organs. The procedure is like ultrasonic cavitation, and it is also a targeted procedure for fat removal. The ultrasonic radiations penetrate beneath the layers of skin without destroying surrounding cells. Extremes heat production will cause the adipose tissue to burn by stimulating collagen formation. This process also promotes the formation of skin collagen due to heat production. The procedure is unique and non-invasive in all ways and does not cause any discomfort. The treatment is also effective as it requires no excision or surgical process. Depending on the volume of fats and fatty tissues, the treatment will continue for months and may last for years.
Conclusion
In conclusion, body sculpting through non-surgical procedures provides the best means for the fatty person to get an attractive body shape without passing through pain and discomfort. Various non-surgical procedures are in use, and body contouring procedures will apply, but depending on the fat reduction goals and the severity of fats, they will apply. There are diverse fat removal methods, depending on which procedure you choose. Non-surgical treatments offer convenient solutions for fat removal, such as ultrasonic techniques, radiotherapies, customized treatment plans, and other high-frequency techniques. Conversely, surgical procedures such as liposuction provide effective results but produce body contouring after a long time, and the procedure is very invasive for every individual. You can reshape multiple organs using the most convenient non-surgical body sculpting methods.